Adenoid cystic carcinoma Definition: Adenoid cystic carcinoma is a malignant tumor arising in the lacrimal gland and is composed of malignant ductular elements.
Incidence/ Prevalence: The most common primary malignant tumor of the lacrimal gland.
Etiology: Unknown but numerous candidate genes have been identified. Increased copy number has been noted at 22q13 for salivary gland adenoid cystic carcinoma. Adenoid cystic carcinoma can arise in benign mixed tumor or de novo in the lacrimal gland.
Clinical Findings: The typical presentation is a 40 year old (median age) with less than 8 months of pain in the upper lateral orbit, numbness, diplopia and proptosis. The tumor is slightly more common in women than in men. The age range is about 8-80 and some authors believe there is a bimodal pattern, the young and the old. The pain symptoms, characteristic of this neoplasm, arise from infiltration of nerves and bone involvement.
Radiology: A rounded mass will generally be centered over orbital portion of the lacrimal gland and the orbital roof may appear moth eaten. This is in distinct contrast from a pleomorphic adenoma. The tumor may extend into the temporalis fossa.
Pathology: Grossly, the appearance is grayish white, firm, and nodular. Under a dissecting microscope the swiss cheese pattern is often quite prominent.
Adenoid cystic carcinoma is not encapsulated. A variety of patterns may appear, including the Swiss cheese (cribriform) pattern.
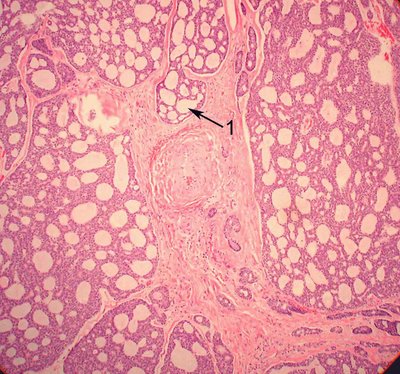
In the image a cribriform pattern is evident with back to back glands without any intervening stroma (arrow 1). This is a sign of adenocarcinoma in general and is a very good distinguishing sign from the ductular structures of the epithelial component of pleomorphic adenoma.
In the upper part of the next image the tumor is forming solid nests indicative of the basaloid type of adenoid cystic carcinoma while below the tumor has a more cylindromatous pattern with glandular elements that are compressed by basement membrane laden and hyalinized stroma.
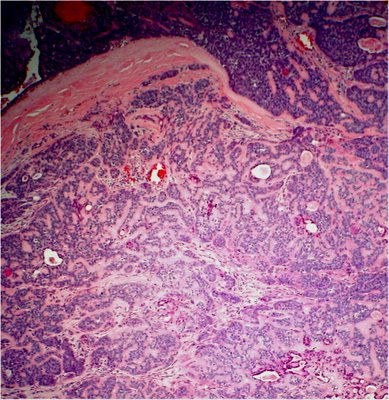
If any of the basaloid pattern is found in an adenoid cystic carcinoma with other predominant patterns, most authors would classify it as a basaloid type with a worse prognosis. Although Lee and Campbell could not verify the worse prognosis in their study at the Mayo clinic, all of their patients with any type of adenoid cystic had generally a worse prognosis than those reviewed in a larger series by Gamel and Font that demonstrate poor survival with the basaloid type of carcinoma. Other histologic patterns include tubular, comedo and sclerosing. Adenoid cystic carcinoma has a proclivity for perineural and occasionally neural invasion.
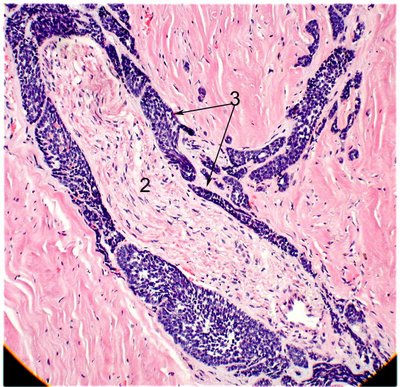
In the image of a basaloid adenoid cystic carcinoma, infiltrating nests of cells (arrow 3) insinuate between the perineurium and the actual nerve fibers (2).
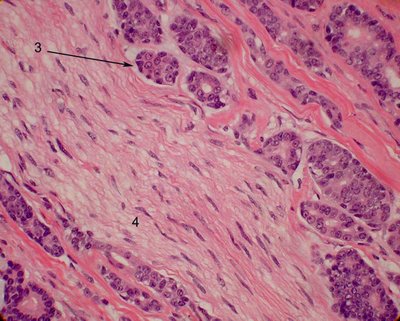
Compare to the more usual cribiform type also exhibiting perineural invasion. The nerve here is shown at number 4.
Treatment: Because of the diffuse infiltration of this tumor, exenteration may be recommended, often with removal of adjacent bone. Anecdotes of aggressive therapy with removal of the lateral wall and the roof of the orbit has been suggested by some as providing a better prognosis and a chance for cure but this has neither been proven, nor borne out in some studies. In general, adenoid cystic carcinoma may recur many times and many years after the initial resection. Intra-arterial cytoreductive chemotherapy has recently been introduced with putatively improved results over conventional therapy.
Prognosis: Despite aggressive surgical intervention, the long-term prognosis is poor. Perineural invasion through the superior orbital fissure to the brain may lead to death. Pulmonary metastases are frequent many years after surgery. Presence of the basaloid pattern has been associated with a worse prognosis (5-year survival of 21%) than those tumors without a basaloid component (5-year survival of 71%).
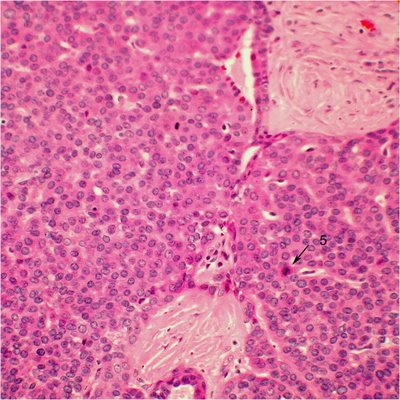
Note the numerous mitotic figures in this image of a basaloid type of adenoid cystic carcinoma (arrow 5).
